Introduction
Recently, lipid nanoparticle (LNP)-based mRNA vaccines have gained widespread attention and offer an attractive modality for personalized cancer therapies. However, inducing an effective anti-tumor response often requires the induction of a T cell response breaking self-tolerance mechanisms, a challenge for current therapies. Providence Therapeutics Holdings Inc. has developed a portfolio of ionizable lipids for the INTENT™ LNP platform. These LNP formulations were carefully screened for their desired end use application. While multiple INTENT™ LNP formulations are capable of inducing expansion of antigen specific T cells, the adjuvant activity of each INTENT™ LNP formulations are distinct. Utilizing an in vivo screening model identifying INTENT™ LNP formulations with adjuvant activity capable of breaking self-tolerance allows the selection of candidates with superior anti-tumor efficacy. In the well characterized mouse syngeneic colorectal cancer (CRC) model expressing model glycoprotein antigens from lymphocytic choriomeningitis virus (LCMV, MC38gp), intramuscular administration of this new INTENT™ LNP formulation as a monotherapy in a therapeutic setting significantly delayedtumor growth and cleared tumors in 50% of treated mice. The data suggests the applicability of our INTENT™ LNP formulations for the development of effective therapeutic mRNA cancer vaccines for multiple solid tumors.
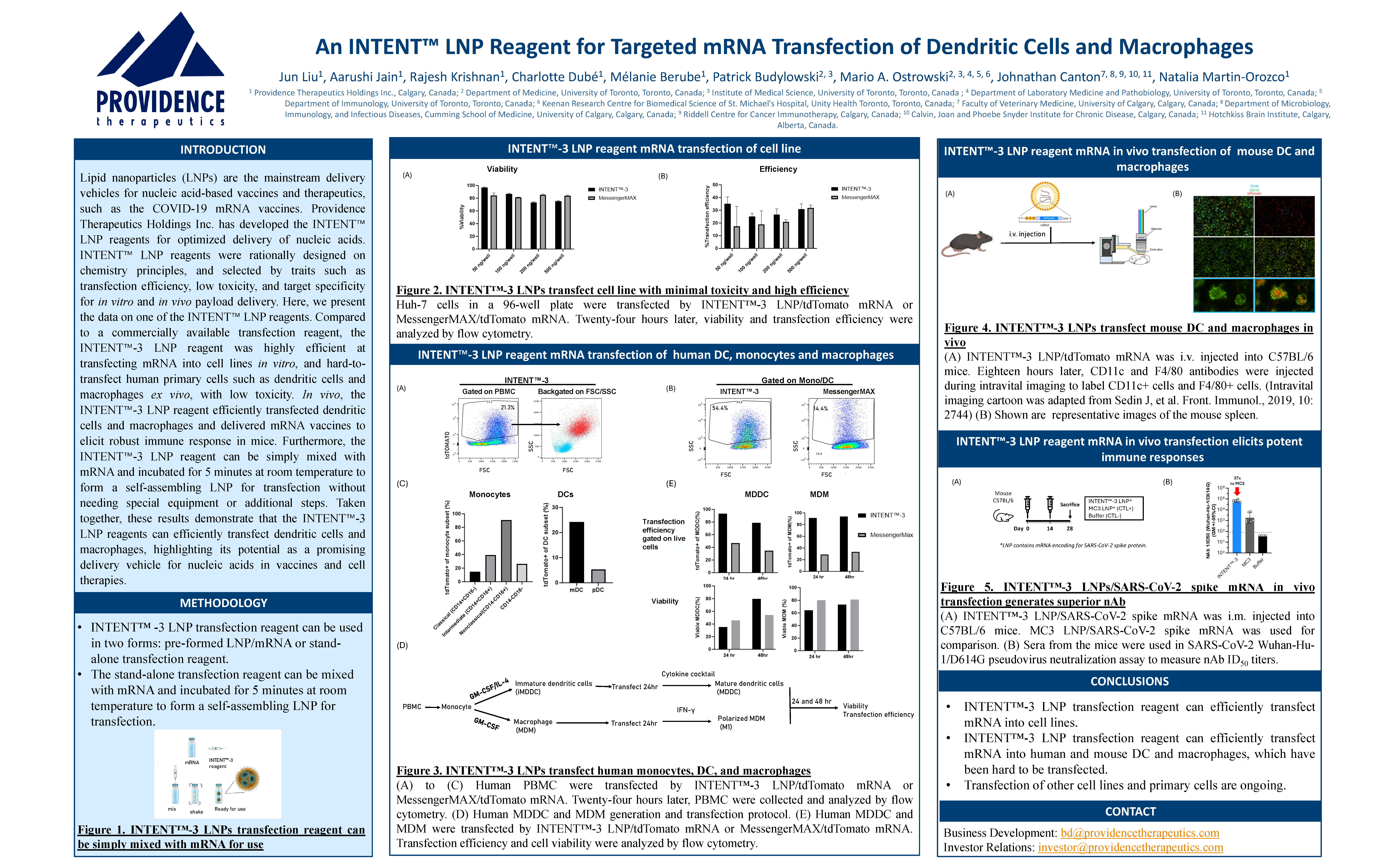
Introduction
Lipid nanoparticles (LNPs) are the mainstream delivery vehicles for nucleic acid-based vaccines and therapeutics, such as the COVID-19 mRNA vaccines. Providence Therapeutics Holdings Inc. Has developed the INTENT™ LNP reagents for optimized delivery of nucleic acids. INTENT™ LNP reagents were rationally designed on chemistry principles, and selected by traits such as transfection efficiency, low toxicity, and target specificity for in vitro and in vivo payload delivery. Here, we present the data on one of the INTENT™ LNP reagents. Compared to a commercially available transfection reagent, the INTENT™-3 LNP reagent was highly efficient at transfecting mRNA into cell lines in vitro, and hard-to-transfect human primary cells such as dendritic cells and macrophages ex vivo, with low toxicity. In vivo, the INTENT™-3 LNP reagent efficiently transfected dendritic cells and macrophages and delivered mRNA vaccines to elicit robust immune response in mice. Furthermore, the INTENT™-3 LNP reagent can be simply mixed with mRNA and incubated for 5 minutes at room temperature to form a self-assembling LNP for transfection without needing special equipment or additional steps. Taken together, these results demonstrate that the INTENT™-3 LNP reagents can efficiently transfect dendritic cells and macrophages, highlighting its potential as a promising delivery vehicle for nucleic acids in vaccines and cell therapies.

Abstract
Lipid nanoparticles (LNPs) are the most studied delivery systems for mRNA therapeutics and have gained importance in both industry and academia following the approval of multiple mRNA-LNP-based vaccines since 2021. The COVID-19 pandemic proved the remarkable efficacy and rapid deployment of mRNA-LNP vaccines, reinforcing their potential for broader therapeutic and vaccine applications. Currently, multiple mRNA-LNPs are in various stages of preclinical and clinical development. LNPs are sensitive to the manufacturing process, and to mitigate the risks associated with bringing an mRNA-LNP from benchtop to industrial scale, it is recommended to have a systematic process development approach, including mathematical modeling and statistical analysis. Among the unit operations required for mRNA-LNP manufacturing, concentration and buffer exchange by tangential flow filtration (TFF), as well as sterile filtration, are challenging and must be optimized to guarantee process scalability and product quality, while avoiding issues such as membrane fouling and incorrect filter capacity. This study investigates the optimization of TFF and sterile filtration parameters to manufacture higher concentration mRNA-LNPs necessary for cancer vaccines, particularly personalized cancer vaccines. Various flat-sheet TFF cartridges were tested under different process parameters, including flow rate and transmembrane pressure (TMP), to identify the most effective process conditions. Furthermore, the sterile filtration of mRNA-LNPs was analyzed using the gradual plugging model, providing insights into improving filter capacity, optimizing filtration pressures, and defining the design space for large-scale manufacturing. These findings contribute to the development of a robust and scalable mRNA-LNP manufacturing process ensuring product quality.

Abstract
The emergence of SARS-CoV-2 variants presents challenges to vaccine effectiveness, underlining the necessity for next-generation vaccines with multiple antigens beyond the spike protein. Here, we investigated a multiantigenic booster containing spike and a chimeric construct composed of nucleoprotein (N) and membrane (M) proteins, comparing its efficacy to a spike-only booster against Omicron BA.5 in K18-hACE2 mice. Initially, mice were primed and boosted with Beta (B.1.351) spike-only mRNA, showing strong spike-specific T cell responses and neutralizing antibodies, albeit with limited cross-neutralization to Omicron variants. Subsequently, a spike-NM multiantigenic vaccine was then examined as a second booster dose for protection in hACE2-transgenic mice. Mice receiving either homologous spike-only or heterologous spike-NM booster had nearly complete inhibition of infectious virus shedding in oral swabs and reduced viral burdens in both lung and nasal tissues following BA.5 challenge. Examination of lung pathology further revealed that both spike-only and spike-NM boosters provided comparable protection against inflammatory infiltrates and fibrosis. Moreover, the spike-NM booster demonstrated neutralization efficacy in a pseudovirus assay against Wuhan-Hu-1, Beta, and Omicron variants akin to the spike-only booster. These findings indicate that supplementing spike with additional SARS-CoV-2 targets in a booster immunization confers equivalent immunity and protection against Omicron BA.5. This work highlights a promising strategy for individuals previously vaccinated with spike-only vaccines, potentially offering enhanced protection against emerging coronaviruses.

Abstract
Continuously emerging SARS-CoV-2 Omicron subvariants pose a threat thwarting the effectiveness of approved COVID-19 vaccines. Especially, the protection breadth and degree of these vaccines against antigenically distant Omicron subvariants is unclear. Here, we report the immunogenicity and efficacy of a bivalent mRNA vaccine, PTX-COVID19-M1.2 (M1.2), which encodes native spike proteins from Wuhan-Hu-1 (D614G) and Omicron BA.2.12.1, in mouse and hamster models. Both primary series and booster vaccination using M1.2 elicited potent and broad nAbs against Wuhan-Hu-1 (D614G) and some Omicron subvariants. Strong spike-specific T cell responses against Wuhan-Hu-1 and Omicron subvariants, including JN.1, were also induced. Vaccination with M1.2 protected animals from Wuhan-Hu-1 and multiple Omicron subvariants challenges. Interestingly, protection against XBB.1.5 lung infection did not correlate with nAb levels. These results indicate that M1.2 generated a broadly protective immune response against antigenically distant Omicron subvariants, and spike-specific T cells probably contributed to the breadth of the protection.

Introduction
Glioblastoma (GBM) is an aggressive primary brain tumor with a dismal prognosis. It is characterized by a limited number of neoantigens and a highly immunosuppressive tumor environment. A well-known GBM-associated driver mutation is EGFRvIII, which is detected in approximately 30% of patients at the time of diagnosis and plays a pivotal role in the emergence of GBM. Its high expression on the tumor cell surface makes it an ideal target antigen for vaccine development, as demonstrated by targeting therapies with antibodies and more recently CAR–T cells.

Introduction
In vitro transcription (IVT) reaction for synthesis of mRNA is commonly performed by adding T7 RNA polymerase (RNAP) and a DNA template. Although the reaction is very efficient, T7 RNAP generates additional immunostimulatory dsRNA impurities – abortive, antisense, and loop-back dsRNAs during the transcription initiation and termination.

Introduction
Lipid nanoparticle(LNP)-based mRNA vaccines have recently gained traction as an attractive modality for cancer therapies. However, inducing an effective anti-tumor response often requires the induction of a T cell response breaking self-tolerance mechanisms, a challenge forcurrent therapies. Providence Therapeutics has developed next-generation LNP formulations, which can break self-tolerance and have the potential to be utilized for therapeutic LNP/mRNA cancer vaccines.

Introduction
Recently, LNP-based mRNA vaccines have gained widespread attention and offer an attractive modality for personalized cancer therapies. However, inducing an effective anti-tumor response often requires the induction of a T cell response breaking self-tolerance mechanisms, a challenge for current therapies.Here, we developed new lipid nanoparticle (LNP) formulations which can be utilized for therapeutic mRNA/LNP cancer vaccines. Utilizing an in vivo screening model identifying LNP formulations capable of breaking self-tolerance allows the selection of LNP candidates with superior anti-tumor efficacy. In the well characterized mouse syngeneic colorectal cancer (CRC) model expressing model glycoprotein antigens from lymphocytic choriomeningitis virus (LCMV, MC38gp), intramuscular administration of this new LNP formulation as a monotherapy in a therapeutic setting after tumor inoculation significantly delayed tumor growth and cleared tumors in 50% of treated mice.
The data suggests the possible applicability of our next generation LNP formulations for the development of effective therapeutic mRNA cancer vaccines for multiple solid tumors.

Introduction
- Glioblastoma (GBM) is the most prevalent and aggressive primary brain tumor type with an abysmal prognosis. a. GBM features an immunologically dampened tumor microenvironment and limited neoantigen production. b. Novel therapeutic strategies for GBM are urgently needed.
- A well-characterized GBM-associated mutation can elicit an anti-tumor immune response: The EGFRvIII mutation.
- The cancer-driver mutation is detected in approximately 30% of patients at the time of diagnosis and plays a pivotal role in the emergence of GBM.
- Its highly immunogenic nature represents an ideal focal point for cutting-edge mRNA-LNP candidate therapeutics.
- (CAR)–T cells directed against EGFRvIII have shown promise in a phase 1 study for GBM treatment, paving the way for a vaccination-based approach.

Abstract
In the aftermath of the COVID-19 pandemic, the evolution of the SARS-CoV-2 into a seasonal pathogen along with the emergence of new variants, underscores the need for dynamic and adaptable responses, emphasizing the importance of sustained vaccination strategies. This observer-blind, double-dummy, randomized immunobridging phase 2 study (NCT05175742) aimed to compare the immunogenicity induced by two doses of 40 μg PTX-COVID19-B vaccine candidate administered 28 days apart, with the response induced by two doses of 30 µg Pfizer-BioNTech COVID-19 vaccine (BNT162b2), administered 21 days apart, in Nucleocapsid-protein seronegative adults 18-64 years of age. Both vaccines were administrated via intramuscular injection in the deltoid muscle. Two weeks after the second dose, the neutralizing antibody (NAb) geometric mean titer ratio and seroconversion rate met the non-inferiority criteria, successfully achieving the primary immunogenicity endpoints of the study. PTX-COVID19-B demonstrated similar safety and tolerability profile to BNT162b2 vaccine. The lowest NAb response was observed in subjects with low-to-undetectable NAb at baseline or no reported breakthrough infection. Conversely, participants who experienced breakthrough infections during the study exhibited higher NAb titers. This study also shows induction of cell-mediated immune (CMI) responses by PTX-COVID19-B. In conclusion, the vaccine candidate PTX-COVID19-B demonstrated favourable safety profile along with immunogenicity similar to the active comparator BNT162b2 vaccine.

Abstract
Access to vaccines against SARS-CoV-2 virus was limited in poor countries during the COVID-19 pandemic. Therefore, a low-cost mRNA vaccine, PTX-COVID19-B, was produced and evaluated in a Phase 1 trial. PTX-COVID19-B encodes Spike protein D614G variant without the proline-proline (986–987) mutation present in other COVID-19 vaccines. The aim of the study was to evaluate safety, tolerability, and immunogenicity of PTX-COVID19-B vaccine in healthy seronegative adults 18–64 years old. The trial design was observer-blinded, randomized, placebo-controlled, and tested ascending doses of 16-µg, 40-µg, or 100-µg in a total of 60 subjects who received two intramuscular doses, 4 weeks apart. Participants were monitored for solicited and unsolicited adverse events after vaccination and were provided with a Diary Card and thermometer to report any reactogenicity during the trial. Blood samples were collected on baseline, days 8, 28, 42, 90, and 180 for serum analysis of total IgG anti-receptor binding domain (RBD)/Spike titers by ELISA, and neutralizing antibody titers by pseudovirus assay. Titers in BAU/mL were reported as geometric mean and 95% CI per cohort. After vaccination, few solicited adverse events were observed and were mild to moderate and self-resolved within 48 h. The most common solicited local and systemic adverse event was pain at the injection site, and headache, respectively. Seroconversion was observed in all vaccinated participants, who showed high antibody titers against RBD, Spike, and neutralizing activity against the Wuhan strain. Neutralizing antibody titers were also detected against Alpha, Beta, and Delta variants of concerns in a dose dependent manner. All tested doses of PTX-COVID19-B were safe, well-tolerated, and provided a strong immunogenicity response. The 40-µg dose showed fewer adverse reactions than the 100-µg dose, and therefore was selected for a Phase 2 trial, which is currently ongoing.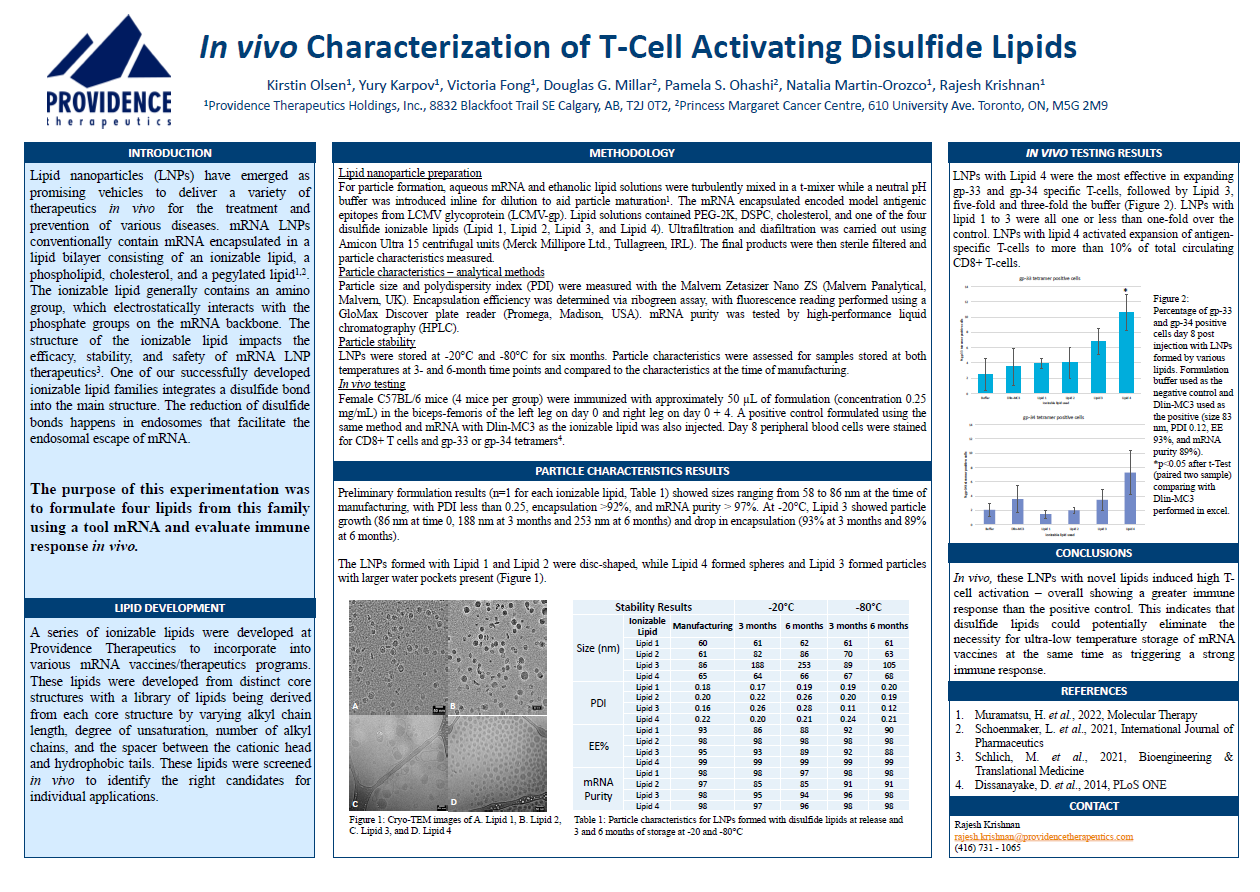
Introduction
Lipid nanoparticles (LNP's) have emerged as promising vehicles to deliver a variety of therapeutics in vivo for the treatment and prevention of various diseases.
mRNA LNPs conventionally contain mRNA encapsulated in a lipid bilayer consisting of an ionizable lipid, a phospholipid, cholesterol, and a pegylated lipid.
The ionizable lipid generally contains an amino group, which electrostatically interacts with the phosphate groups on the mRNA backbone. The structure of the ionizable lipid impacts the efficacy, stability, and safety of mRNA LNP therapeutics. One of our successfully developed ionizable lipid families integrates a disulfide bond into the main structure. The reduction of disulfide bonds happens in endosomes that facilitate the endosomal escape of mRNA.

Abstract
Safe and effective vaccines are needed to end the COVID-19 pandemic. Here, we report the preclinical development of a lipid nanoparticle–formulated SARS-CoV-2 mRNA vaccine,
PTX-COVID19-B. PTX-COVID19-B was chosen among three candidates after the initial mouse vaccination results showed that it elicited the strongest neutralizing antibody response against SARS-CoV-2. Further tests in mice and hamsters indicated that PTX-COVID19-B induced robust humoral and cellular immune responses and completely protected the vaccinated animals from SARS-CoV-2 infection in the lung. Studies in hamsters also showed that PTX-COVID19-B protected the upper respiratory tract from SARS-CoV-2 infection.
Mouse immune sera elicited by PTX-COVID19-B vaccination were able to neutralize SARS-CoV-2 variants of concern, including the Alpha, Beta, Gamma, and Delta lineages. No adverse effects were induced by PTX-COVID19-B in either mice or hamsters. Based on these results, PTX-COVID19-B was authorized by Health Canada to enter clinical trials in December 2020 with a phase 2 clinical trial ongoing.